Sex influences the heart 💜
Literally, I'm not being romantic or lyrical here.
Patients' gender-related characteristics may partly explain traditional sex differences in risk factors for cardiovascular disease (such as for acute coronary syndrome).
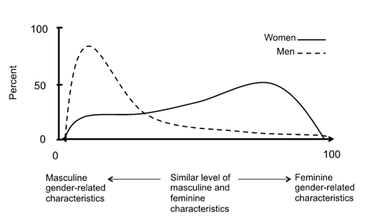
The graph below shows that sex and gender are partly independent (which means, not totally separate but also not the same thing). Additionally, individuals with high feminine gender scores were twice as likely to be re-admitted to hospital and to experience worse prognoses following discharge after heart attack.
Now, I'm not saying that men act all tough in the presence of male doctors... but they do. Nor am I saying that birthing mothers feel more at ease to scream in pain when a female doctor pops in... but they do.
So, how representative are studies in animals and what can we learn from them?
The male observer effect — mice and rats exposed to painful stimuli displayed less discomfort when the experimenter was male compared to a female. This response seems to depend on olfactory stimuli: male rodents experienced physiological stress when smelling other males (humans, in this case), which dampened the intensity of the perceived pain.
The nervous system and immune systems are both involved in the development, maintenance, and control of chronic pain.
In experiments with male and female mice, injuries to peripheral nerves caused an increased sensitivity to pain. While T lymphocytes (white blood cells) mediated the response in female mice, in males the response depended on microglia (which are central nervous system cells). However, pregnant female mice switched to the male-typical pathway, while male mice that lacked testosterone switched to the female-typical pathway. This is because testosterone activates microglia and suppresses T cells, while estrogens activate T cells.
If this is confirmed to be the same in humans, it could lead to the development of female and male-specific painkillers, and affect treatment choices in patients undergoing hormone therapy. Nevertheless, if pain signaling is different in men and women, so are the perception and expression of pain that lead to marked gender differences in treatment-seeking behaviour and drug prescriptions.
It's important to keep in mind that even symptoms and diagnosis criteria for heart disease often differ between men and women. When adjusted for age, ethnicity, income, education, sex assigned at birth, and self-reported gender identity, the impact that gender constructs have on self-rated health (both physical and mental) are critical. Gendered differences are flagrant in caregiver strain, work strain, independence, risk-taking, emotional intelligence, social support, and discrimination.
 |
| Gendered Innovation in Health and Medicine |
Understanding and acceptance that differences unite us girls and boys rather than set us apart is essential. For pain and heart health... it takes a village.



Comments
Post a Comment